CASE REPORT | https://doi.org/10.5005/jp-journals-10031-1269 |
Persistent Oral Infection Caused by an Iatrogenic Displacement of a Lower Third Molar Root to the Sublingual Space
1,4,5School of Dentistry, University Centre of Para–CESUPA, Belem, Pará Brazil
2,3,6,7School of Dentistry, Federal University of Pará (UFPA), Belém, Pará, Brazil
Corresponding Author: João de Jesus Viana Pinheiro, School of Dentistry, Federal University of Pará (UFPA), Belém, Pará, Brazil, Phone: +55 91 989776543, e-mail: radface@hotmail.com
How to cite this article Sousa NWA, de Moraes ATL, Guimarães DM, et al. Persistent Oral Infection Caused by an Iatrogenic Displacement of a Lower Third Molar Root to the Sublingual Space. J Contemp Dent 2019;9(3):155–158.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Aim and objective: Describe a case of sublingual displacement of a root of the lower third molar, as well as highlight the importance of using appropriate complementary imaging tests and provide the clinician with information on how to prevent and treat this complication.
Background: The displacement of the lower third molar is an accidental event that can lead to serious complications, which is usually the cause of inadequate surgical technique.
Case description: A 69-year-old man presented pain and trismus due to local infection 1 month after a tooth extraction. After a misdiagnosis of retained root and surgical exploration, a cone-beam computed tomography (CBCT) showed a displaced root into the sublingual tissues. A surgical procedure under local anesthesia was carried out to easily remove the displaced tooth root, which resulted in complete healing of soft tissues and disappearance of signs of local infection.
Conclusion: The use of CBCT is essential for the identification and location of the dislocated tooth and the removal of the fragment, as it allows a three-dimensional assessment providing adequate surgical planning which resulted in complete remission of all symptoms.
Clinical significance: Few reports have been published to describe this rare complication of dental extractions that support key points for proper management: (1) the use of three-dimensional imaging for proper evaluation and establishment of exact location; (2) careful surgical planning; (3) precise surgery. Successful tooth removal is the main goal of treatment, which usually results in control of associated signs and symptoms.
Keywords: Case report, Oral infection, Oral surgery, Retained root, Tooth displacement..
BACKGROUND
Removal of third molars is one of the most common surgical procedures in dentistry, which are routinely performed by either general dentists and oral and maxillofacial surgeons.1 Despite being commonly performed in dental offices, surgical removal of third molars is considered technically difficult,2 and complications during and after their removal are frequently reported.3–7 The most common complications are listed as pain, dry socket, swelling, paresthesia of the lingual or inferior alveolar nerve, bleeding, and infection.4 Displacement of the entire lower third molar or its fragments are uncommon complications and can be very challenging of diagnosing and treating, especially when there is no previous information about this surgical accident.
Atypical anatomic location of lower third molars can increase the difficulties of surgical removal and the risks of tooth displacement. However, in most cases, displacement of the lower third molars is due to improper surgical technique or uncontrolled power.5 Symptoms of tooth displacement are nonspecific and can include pain, swelling, trismus, infection, and further migration of the root or root fracture even into deep spaces.3–7
In a few cases, displacement of lower third molar can be asymptomatic, and removal of the displaced tooth or fragment cannot be necessary. However, symptoms are present, treatment consist of a proper localization and surgical removal.3–6 The removal of the tooth or fragment can be very challenging and its localization into soft tissues is difficult because of migration and tissue movement during manipulation.4–6
This study reports a very rare case of a small root fragment of a lower third molar into the sublingual space. Diagnosis was complicated because the patient was not informed of any complications during the third molar surgery and the difficulties of proper localization on panoramic radiography.
CASE DESCRIPTION
A 69-year-old man was referred to our clinic for multiple tooth extractions. On his first appointment, the patient reported trismus and pain on his right mandible 1 month after the extraction of 48. He reported that the surgical procedure appeared to be normal and uneventful, and the dentist did not communicate him of any accident. The patient who appears on the images has signed an informed patient consent authorizing the publication of his images.
Clinically, the patient presented a fistula on the alveolus of the lower third molar with drainage of pus (Fig. 1A). Amoxicillin was prescribed for 1 week and a panoramic radiography was taken that showed an image suggesting a retained lower third molar root and signs of sclerosing osteomyelitis (Figs 1B and C). A surgical procedure was carried out to explore the dental socket and to remove the residual root. However, the dental socket was empty without any apparent cause for the persistent infection.
The patient evolved with a temporary improvement of symptoms and a cone-beam computed tomography (CBCT) was requested. Meanwhile, the other teeth were removed, which included all remaining maxillary teeth (16, 15, 14, 11, 21, 22, and 24) and two residual mandibular roots (32 and 34) (Fig. 1D). The CBCT showed an alteration on the mandibular bone trabeculae with sclerosis around the alveolus of the 48, and an image suggestive of a tooth fragment lingually displaced on the lingual region (Figs 2A to C).
Another surgery was planned under local anesthesia that included an incision over the mandibular body and a relaxing lingual incision anteriorly. A subperiosteal flap was performed and the lingual soft tissues were retracted. After careful exploration with a Molt dissector, a hard tissue in the sublingual region was felt with the dissector tip. Then, a controlled dissection exposed the root fragment, which was easily removed after its identification (Fig. 2D). The wound was surgically closed and amoxicillin (7 days) and nonsteroid anti-inflammatory (4 days) were prescribed postoperatively. The patient evolved very well, the wound healed appropriately, without any signs of local or systemic infection.
DISCUSSION
Accidental displacement of a third molar or root fragment during surgical extraction is rare, and complications are commonly observed after these events.3–10 The most common sites of dislodgment of an impacted mandibular third molar fragment are the sublingual, submandibular, and pterygomandibular spaces. Removal of a displaced root tip from these spaces may be complex due to poor visualization and limited access. A thorough evaluation of all significant risk factors must be performed in advance to prevent complications.
Before extraction of mandibular molars, the degree of impaction, root position, distal inclination, and bone density should be evaluated, in order to minimize possible accidents during the surgical procedure.
In addition, if necessary, adequate surgical access should be planned. The elevation of the mucoperiosteal flap to obtain adequate exposure of the surgical field coupled with an appropriate instrumentation and providing the amount and direction of force that is deserved is of great importance for the success of the procedure.10
Here, we described a case that a small root fragment was displaced to the sublingual space and the patient was not informed of this accident to his dentist, which could be due to lack of experience/technical skills who did not notice the accidental displacement, or because he was afraid of legal problems. This attitude is unappropriated and the literature recommends that patients should be promptly informed about this type of accident.7
After an initial uneventful postoperative period, pain and trismus developed and the patient sought for further assistance. Since the patient was unaware of any complication during the removal of his 48, a proper diagnosis was delayed.
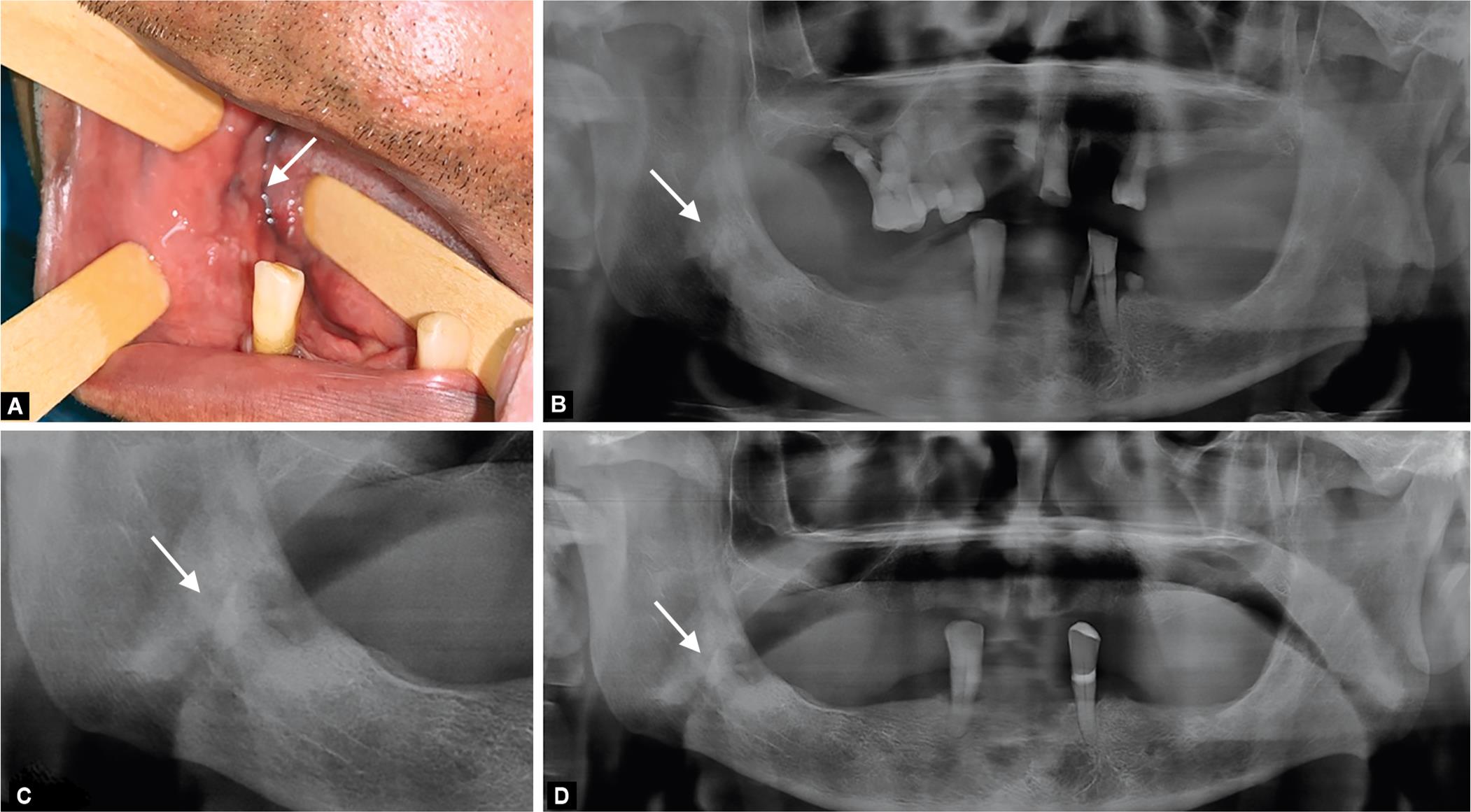
Figs 1A to D: Clinical appearance showing an oral fistula (white arrow) on the mandible (A). Panoramic radiography on admission (B), and post dental extractions (C and D), showing sclerosing osteomyelitis and an image suggestive of a retained dental root (white arrow)

Figs 2A to D: (A) 3D CBCT reconstruction showing the displaced root; (B) Root fragment measuring 10 x 6 mm; (C) CBCT coronal cut showing the root location; (D) Removed dental root and fistula. Dental root is indicated by the white arrow
Complications took 1 month to appear, which could lead to a serious infection since the contaminated root was already located into the lingual space and infection could easily spread to other deep fascial spaces and a life-threatened infection could develop.
Accurate diagnosis and treatment planning are the backbone of any surgical procedure; for this reason, imaging tests are important complementary techniques to arrive at a definitive diagnosis. In view of this, it is a fact that panoramic radiography is the routine imaging exam used for planning uncomplicated dental extractions. However, its two-dimensional image limits the information necessary for planning complex and/or complicated cases, such as the one presented.4–6
Conical beam computed tomography has been introduced and has been widely used. Its technology provides a three-dimensional image visualization, allowing the exact location and extension of any anatomical region. For the situation presented in this report, the three-dimensional assessment using the CBCT was essential for proper diagnosis and surgical planning, resulting in a good postoperative for the patient.
In summary, in this study, we describe a very rare case of displacement of the root of the lower third molar to the sublingual space that was diagnosed late after the development of pain and trismus. The patient was unaware of the accidental displacement of his tooth root during the removal of the lower third molar, which led to the development of local infection, delayed diagnosis and treatment, and misguided the unsuccessful exploration of the tooth socket due to the limited information provided by the patient/dentist reference and panoramic radiography. The use of CBCT is highly recommended, and provided us with an accurate location of the root, assisting in the proper surgical planning, and it was fundamental for the successful removal of the dental fragment. There were no postoperative complications.
CONCLUSION
Accidental displacement of a root from the lower third molar to the sublingual space is an uncommon complication that can lead to severe complications. Therefore, an adequate clinical and radiological evaluation must be performed. If a dental fragment is moved into a deep space, it is very important to determine the exact location, for which it is recommended to use high quality imaging exams, as is the case with CT scans.
CLINICAL SIGNIFICANCE
Few reports have been published to describe this rare complication of dental extractions that support key points for proper management: (1) the use of three-dimensional imaging for proper evaluation and establishment of exact location; (2) careful surgical planning; (3) precise surgery.3–8 Successful tooth removal is the main goal of treatment, which usually results in control of associated signs and symptoms.
ETHICAL APPROVAL
We declare that our institution does not require ethical approval of clinical case reports.
REFERENCES
1. Cunha-Cruz J, Rothen M, Spiekerman C, et al. Recommendations for third molar removal: a practice-based cohort study. Am J Public Health 2014;104(4):735–743. DOI: 10.2105/AJPH.2013.301652.
2. Sebastiani AM, Todero SRB, Gabardo G, et al. Intraoperative accidents associated with surgical removal of third molars. Braz J Oral Sci 2014;13(4):276–280. DOI: 10.1590/1677-3225v13n4a07.
3. Nusrath MA, Banks RJ. Unrecognised displacement of mandibular molar root into the submandibular space. Br Dent J 2010;209(6):279–280. DOI: 10.1038/sj.bdj.2010.816.
4. Deliverska EG, Petkova M. Complications after extraction of impacted third molars - literature review. J IMAB - Annu Proceed (Scientific Pap) 2016;22(3):1202–1211. DOI: 10.5272/jimab.2016223.1202.
5. Jolly SS, Rattan V, Rai SK. Intraoral management of displaced root into submandibular space under local anaesthesia - a case report and review of literature. Saudi Dent J 2014;26(4):181–184. DOI: 10.1016/j.sdentj.2014.05.004.
6. Flygare L, Öhman A. Preoperative imaging procedures for lower wisdom teeth removal. Clin Oral Investig 2008;12(4):291–302. DOI: 10.1007/s00784-008-0200-1.
7. Anand R, Patil PM. Accidental displacement of third molars; Report of three cases, review of literature and treatment recommendations. Oral Surg 2013;6(1):2–8. DOI: 10.1111/ors.12013.
8. Tamer Y, Pektas ZO. Accidental displacement of mandibular third molar roots into the pterygomandibular space. Niger J Clin Pract 2018;21(8):1075–1077. DOI: 10.4103/njcp.njcp_427_17.
9. Jain A. Accidental displacement of mandibular first molar root into buccal space: a unique case. J Stomatol Oral Maxillofac Surg 2018;119(5):429–431. DOI: 10.1016/j.jormas.2018.04.004.
10. Aznar-Arasa L, Figueiredo R, Gay-Escoda C. Iatrogenic displacement of lower third molar roots into the sublingual space: report of 6 cases. J Oral Maxillofac Surg 2012;70(2):107–115. DOI: 10.1016/j.joms.2011.09.039.
________________________
© The Author(s). 2019 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.